Defining Pain
Medical Definition: Pain is often defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.
Subjective Nature of Pain Perception: Pain is highly subjective and varies from person to person.
Differentiating Types of Pain: Acute pain is short-lived and typically a result of injury, while chronic pain persists beyond the expected healing time.
The Physiology of Pain
Nervous System’s Role: Pain signals are transmitted through the nervous system, from specialized nerve endings to the brain.
Neurotransmitters: Chemical messengers in the brain, such as endorphins and serotonin, play a role in pain perception.
Brain Regions: Areas like the thalamus and cortex process and interpret pain signals.
Factors Influencing Pain Perception
Psychological Factors: Emotions and expectations can influence how we perceive pain.
Sociocultural Influences: Cultural attitudes towards pain can impact individual experiences.
Environmental Context: External factors like noise or lighting can affect pain perception.
Types of Pain
Nociceptive Pain: Arises from damage to tissues and is typically sharp and localized.
Neuropathic Pain: Caused by nerve damage and may present as burning or shooting pain.
Psychogenic Pain: Without identifiable physical cause, often related to psychological factors.
The Impact of Pain
Physical Effects: Chronic pain can lead to fatigue, weakened immune system, and sleep disturbances.
Emotional and Psychological Consequences: Pain can contribute to anxiety, depression, and decreased quality of life.
Social and Functional Implications: Pain may limit daily activities and affect relationships with others.
Assessing and Diagnosing Pain
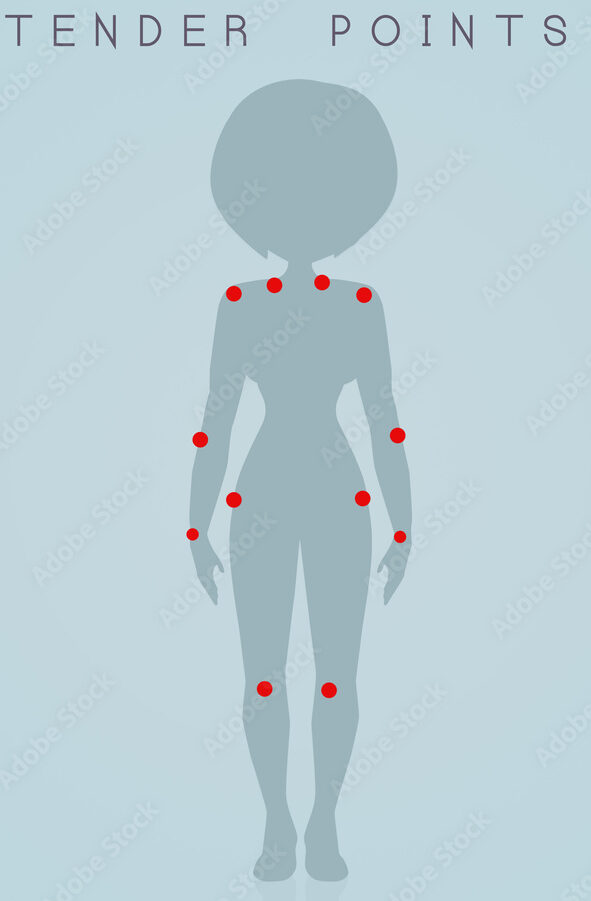
Patient History: Understanding the nature of pain through patient-reported measures is crucial.
Objective Assessments: Diagnostic tools like imaging studies can help pinpoint the source of pain.
Multidisciplinary Approaches: Involving various healthcare professionals in pain diagnosis leads to a comprehensive evaluation.
Treatment and Management Strategies
Pharmacological Interventions: Medications like analgesics and anti-inflammatories target pain relief.
Non-Pharmacological Approaches: Physiotherapy and cognitive-behavioral therapy can complement conventional treatments.
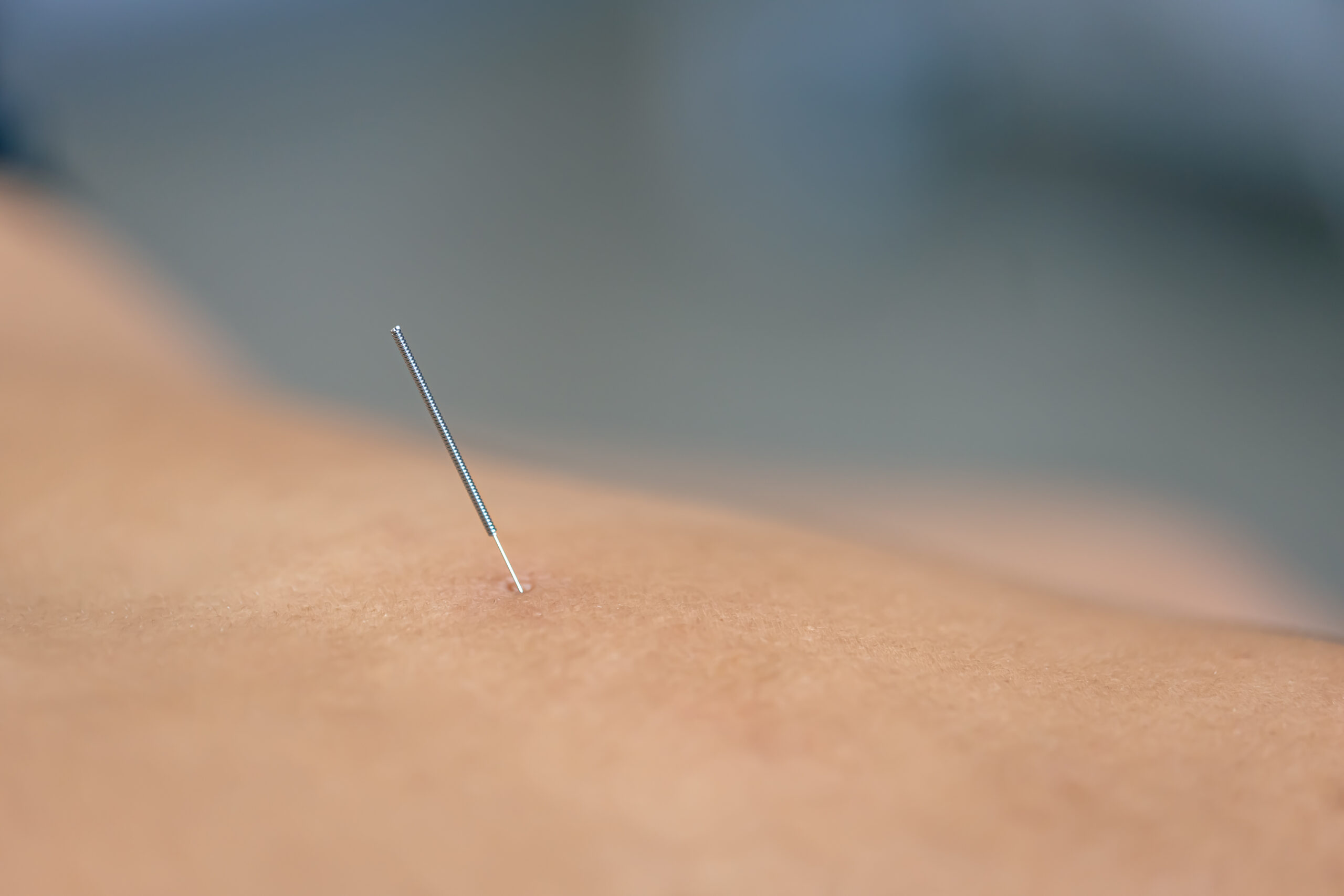
Integrative Medicine: Techniques like acupuncture and yoga offer holistic pain management options.
Pain Education and Empowerment
Patient Education: Providing information on pain mechanisms and management strategies empowers individuals.
Self-Management Techniques: Teaching coping strategies and self-care practices enhances patient autonomy.
Advocacy for Patient-Centered Care: Fostering a partnership between healthcare providers and patients promotes personalized pain management.
Conclusion
- Recapitulating the multifaceted nature of pain underscores the importance of a comprehensive approach to pain management.
- Emphasizing the need for ongoing research and advancements in pain treatment for better patient outcomes.